An article published in June 2020 by Dr. Benjamin Lok et al beautifully summarizes not only the nature of small-cell lung cancer (SCLC), but the three major preclinical models used in various studies during the development of novel therapeutic methods. First off, we need to remember some facts about the disease itself: SCLC comprises about 15% of all lung cancer cases. It also has a high mortality rate with a <10% 5-year survival rate. This is because even though the initial tumor may have up to a 70% response rate to treatment, the disease will come back quickly and will have adapted to resist the previous treatment used.
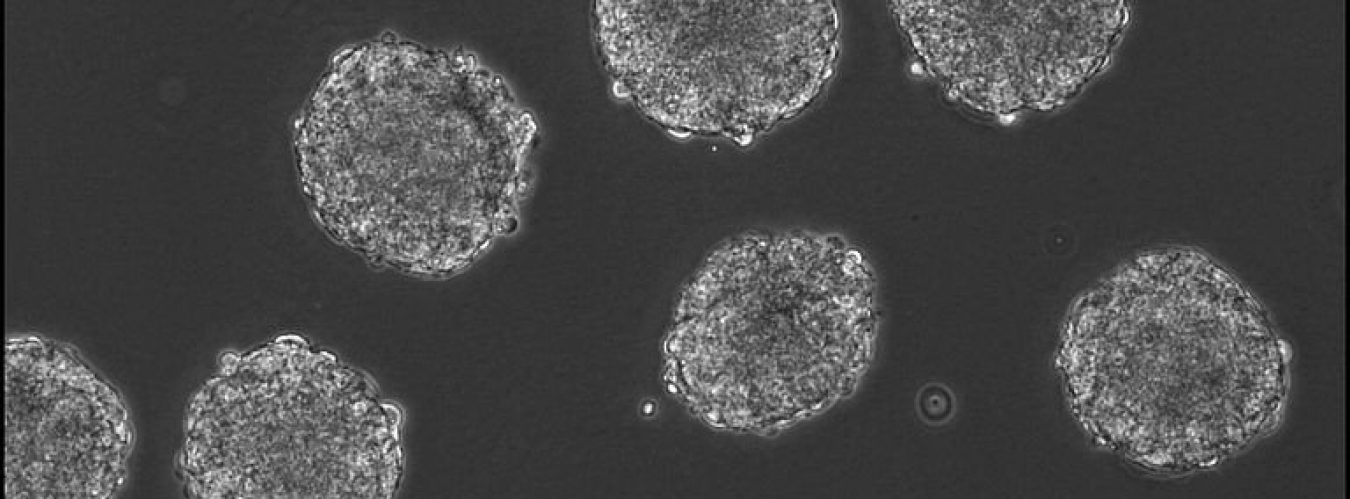
With this in mind, three different SCLC models are being used to find more effective treatments. The first one discussed is two-dimensional cell cultures, which use immortalized cell lines. In layman’s terms, this means that the cells growing in the dish can continue dividing over and over again, continually making more. One of the more famous examples of an immortalized cell line is HeLa cells, derived from cervical cancer cells in 1951. (A topic for another article.) The advantages of this model are that it’s cost-effective, relatively fast, and easy to handle. However, because growing flat on a dish (in vitro) does not replicate the conditions a tumor encounters in a body, these cells don’t express the same genes. So, these studies don’t usually lead to successful clinical drug development. The second model used is cancer cell line xenografts, which are immortalized human cancer cells that are implanted into mice with compromised immune systems (immunodeficient). Although these cells are growing in a living body (in vivo), they still don’t entirely replicate the gene expression patterns in primary tumors (the tumors actually in the patients, which can have cells taken directly from them via biopsy, but more on that snag later.). These cells also don’t have the diverse mixture of genetic expression found in primary tumors either because that gets lost when culturing a cell line. So, this option is a bit better than 2D cell culture, but still not perfect. The third model option, which seems to show the most promise, is patient-derived xenographs (PDX). These are cells taken directly from a patient’s tumor and placed in immunodeficient mice. After the cells have a few weeks to adjust to their new home, they can be sequenced and used to test various therapies. These PDX models preserve the heterogenous gene expression patterns and respond very similarly to drugs. These correlate significantly to clinical outcomes. Here’s the catch: not all primary tumors can be established as xenografts. Also, passaging (transferring cells between dishes) can change their genetic expression profiles. Lastly, because the mice are immunodeficient, the immune system doesn’t really do much of anything with the tumor cells. So, we cannot completely model the complex interactions between a tumor and its environment, which makes it harder to develop novel immunotherapies. However, this last disadvantage can be addressed by using humanised mice. These mice are immunodeficient like their other friends, but engrafted (injected) with human hematopoietic (blood cell-making) stem cells that develop into functional human immune cells to be used in immuno-oncology studies. With these new models in mind, progress continues to march forward. I hope that everyone learned something new today!
Here is the article for those interested in more detail:
https://www.clinicaloncologyonline.net/article/S0936-6555(20)30227-2/fulltext